Looking Beyond Symptoms: How Ergonomics Can Help Fight the Opioid Epidemic
03/06/2020

In recent years, there has been a great deal of justified concern about the abuse of prescription opioids. The National Institute on Drug Abuse states that every day, 128 people in the US die from opioid overdoses, and the total economic burden of prescription opioid misuse totals $78.5 billion per year. Even so, most discussion of opioids focuses on recognizing and treating signs of addiction and improving access to alternate pain treatments, rather than addressing the underlying reasons for such widespread use.
It’s a foregone conclusion that people often begin using pain-management drugs like opioids because they experience pain, and a significant number of all opioid prescriptions are due to work-related injuries.
Here, we’ll take a look at the underpinnings of the opioid epidemic, and examine the evidence of connections between poor workplace ergonomics and chronic pain.
Anatomy of an Epidemic
The roots of the current opioid epidemic likely go back to about 1995, when the synthetic opioid OxyContin entered the pharmaceutical market. Medical practitioners promoted a view of pain as “the fifth vital sign” at this time, and focused more attention on pain and its treatment. This school of thought helped lay the groundwork for more aggressive use of prescription opioids for chronic pain.
As a result, opioid prescription sales to hospitals, pharmacies, and practitioners nearly quadrupled in the US between 1999 and 2010. Annual rates of opioid prescriptions also increased from 72.4 per every 100 persons in 2006 to 80 per 100 persons in 2012.
With these higher rates of opioid prescriptions came additional problems. National Institute of Health (NIH) data indicates that 21 to 29 percent of patients prescribed opioids for chronic pain misuse them, and roughly 8 to 12 percent develop an opioid use disorder. Additionally, some prescription opioid users also report using heroin due to either its lower cost relative to prescription opioids or more intense narcotic effects. Between 4 to 6 percent of those who misuse prescription opioids also use heroin, and four out of five heroin users report using prescription opioids first.
The consequences have been catastrophic. According to the Centers for Disease Control and Prevention (CDC), opioid overdoses killed more than 47,600 people in 2017, more than any previous year on record, with 37% of those deaths involving prescription opioids. Additionally, 95% of overdose fatalities occurred among working aged persons 15 to 64 years old.
MSDs and Chronic Pain
That last statistic begs the question whether there may be a connection between workplace injuries and rates of opioid addiction. Recent data from several sources point to exactly such a connection.
Information released by the Utah Department of Health, the Office of Medical Examiners and the Labor Commission of Utah in 2019 indicates that 57 percent of Utah residents who died from opioid-related overdose deaths had at least one prior workplace musculoskeletal disorder (MSD). 13 percent had experienced a work-related injury within three years of their death.
Additionally, multiple sources indicate that the highest rates of opioid-related overdose fatalities occur in physically demanding industries requiring repeated forceful exertions. For example, data released by the Massachusetts Department of Public Health indicates that the highest rates of overdoses occurred in industries such as construction, forestry, material moving, installation and repair, food preparation and service, building maintenance and healthcare.
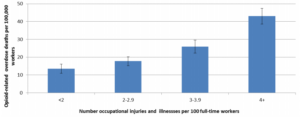
The Massachusetts study provides additional evidence of a link between occupational injuries and opioids by exploring how rates of opioid-related deaths vary based on work-related injury and illness rates as provided by the 2015 Survey of Occupational Injuries and Illnesses published by the Bureau of Labor Statistics (BLS). The figure below summarizes the results. As shown, workers in industry sectors with fewer than 2 injuries/illnesses per 100 full-time equivalent workers had the lowest rate of opioid overdose deaths, while workers in industries with more than 4 injuries/illnesses per 100 workers had the highest rates.
We can gain additional insights from these numbers if we remember that various other studies have documented the frequency of opioid prescriptions for pain management following a workplace injury. For example, a 2011 metareview of studies found that an average of 32 percent of injured workers received opioid prescriptions, and the National Council on Compensation Insurers reported that 25 percent of worker’s compensation drug claim costs in 2011 were for opioid pain medications.
Data suggests that worker’s compensation systems and policies have actually contributed to the opioid problem. For example, data provided by the National Council on Compensation Insurance (NCCI) shows that in 2016, injured workers who were prescribed with opioid medication received three times as many prescriptions as the average US prescription rate. In 2016, 44 percent of all worker’s compensation claims with prescriptions included at least one prescription for opioids. 15 percent of those prescriptions were related to occupational injuries going back six or more years.
This last statistic points us to another key contributing factor — that workers who receive opioid prescriptions tend to keep using the drugs for an extended period of time. A 2018 cohort study of 9,596 worker’s compensation claimants who were prescribed to opioids found that 30% of claimants continued to fill opioid prescriptions more than 90 days after their injuries.
MSDs are one of the most common injuries worldwide. They are currently the second greatest cause of disability globally, accounting for 31 percent of all occupational injuries and illnesses in the US, and 50 percent of all injuries in Canada. Because MSDs often result in chronic pain, they are exactly the kind of injuries for which workers would likely receive opioid prescriptions.
So, let’s put it all together and summarize our key conclusions:
- Based on the information we’ve reviewed, workplace injuries commonly result in prescriptions for opioids — especially within workers’ compensation frameworks
- Among all workplace injuries, MSDs are one of the most common, and are also highly likely to result in an opioid prescription
- One study showed that the majority of workers who died from opioid overdoses had at least one prior MSD
- Injured workers prescribed to opioids receive more prescriptions compared to members of the general public, and maintain those prescriptions for longer periods of time
- At least some of those individuals also transition to heroin use
- Finally, the rate of opioid-related fatalities shows a direct correlation with rates of workplace injuries and illnesses, suggesting a direct causal link between workplace injuries and opioid use.
What Can We Do?
The data presented here certainly suggests that preventable work-related MSDs play a role in contributing to the opioid epidemic. Fortunately, there are steps we can take today to address this critical problem.
One strategy should be to significantly reduce the number of opioid prescriptions given to our workers in response to workplace injuries. There are two compelling reasons for this:
First, opioids simply don’t work well enough to merit their current “first resort” status. A 2018 study found essentially no difference in improvement between a group of patients treated for chronic pain using opioids, and another group treated with non-opioid medications. Many other studies report similar findings.
Second, opioid prescriptions are linked with prolonged pain and disability. One study conducted by the California Worker’s Compensation Institute revealed that injured workers who received high doses of opioid painkillers stayed off work three times longer than those with similar injuries who took smaller doses. This results in longer and more costly workers’ compensation claims. For more information on better ways to manage MSDs, check out our e-book Five Approaches to Managing MSDs: What Really Works.
The most impactful action we can ultimately take is to prevent injuries in the first place. MSDs are one of the most significant causes of chronic pain, but we can effectively prevent MSDs by planning and implementing workplace ergonomics programs.
Whether you’re in an office environment, industrial environment or both, we all encounter ergonomics stressors in the workplace. Many jobs require physical exertion, involve repetitive motion, or introduce the potential for strains and overexertion due to suboptimal design. Repeated exposure to these stressors can eventually cause the development of MSDs including carpal tunnel syndrome, tendonitis and lower back disorders, all of which can create the kind of chronic pain that has historically resulted in increased use of prescription painkillers.
With an active ergonomics program that involves and addresses the entire workforce, we can recognize when these stressors are present and remove them before they can cause MSDs. We can break the chain that leads to opioid prescription at the first link, and prevent chronic pain from ever developing in the first place. Luckily, modern ergonomics software makes this easier than ever to do.
With the right tools, we can help stop the opioids epidemic while simultaneously create a safer and more productive workplace.
Let VelocityEHS Help!
Our HumanTech Ergonomics solutions give you and your workforce powerful tools for identifying and eliminating ergonomics stressors, and includes innovative features like A.I. motion-capture technology, online training and assessment tools, and a centralized database to make managing workplace ergonomics faster, easier and more cost effective.
Whether you’re looking for help managing office or industrial ergonomics, we can give you the support you need. Contact us today to learn more about how we can help you.