Simplifying OSHA’s Respiratory Protection Standard: Part 1
10/16/2019

Since 2009, OSHA’s Respiratory Protection Standard has consistently ranked fourth on the agency’s annual Top 10 List of Most Frequently Cited Standards. Despite the wealth of OSHA guidance and compliance resources available to employers, not to mention an entire industry dedicated to respiratory PPE, air quality monitoring and engineering control technologies, it’s clear that many employers continue to struggle with respiratory protection in the workplace.
In this two-part VelocityEHS Blog series, we’re going to zero-in on OSHA’s Respiratory Protection Standard to help simplify the requirements for covered employers, outline the key challenges to compliance, and introduce some essential best practices employers can implement to more easily and effectively manage respiratory protection in the workplace.
Register Today for our upcoming webinar to view a live product demo of our IH solution and see for yourself just how simple IH program management can be with VelocityEHS!
Respiratory Protection: A Matter of Life & Death
NIOSH National Occupational Respiratory Mortality System (NORMS) data shows that between 2006 and 2016, 51,822 U.S. residents died from occupational-related respiratory illnesses. That’s an average of more than 5,000 each year. In 2016 alone, occupational-related respiratory illnesses took the lives of 4,500 Americans. That’s nearly equal to the total number of U.S. workers killed on-the-job during that same year (5,190). That makes occupational respiratory illness the single greatest cause of occupational fatalities.
These numbers can be a little confusing. To help clear things up, we first need to draw the distinction between on-the-job fatalities versus occupational-related fatalities. Respiratory exposure to harmful substances rarely results in immediate, on-the-job fatality. In fact, the BLS Census for Fatal Occupational Injuries (CFOI) 2011-2017 shows that in 2016, inhalation of harmful substances resulted in just 39 of the 5,190 on-the-job fatalities recorded that year. For comparison, the CFOI showed that the most common cause of on-the-job fatalities in 2016 was transportation-related incidents which resulted in 2,083 worker deaths. Sadly, it is almost always the case that occupational respiratory mortality is due to years of repeated exposures that eventually result in chronic, terminal respiratory illnesses like silicosis, mesothelioma, pneumoconiosis and other lung diseases. By the time workers are aware of their symptoms, it’s often too late.
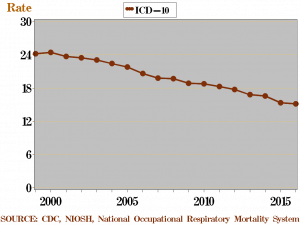
Thankfully, major revisions to OSHA’s Respiratory Protection Standard introduced in 1998 have helped to gradually lower the rate of fatal occupational respiratory illness from greater than 24 per 100,000 workers pre-1998, to around 15 per 100,000 workers by 2016.
Unfortunately, the continued diagnosis of serious and often fatal occupational respiratory illnesses, as well as the persistence of Respiratory Protection Standard violations on OSHA’s Top 10 List make it clear that employers still have a long way to go when it comes to protecting worker health and safety.
Breaking Down OSHA’s Respiratory Protection Standard
OSHA’s Respiratory Protection Standard is one of the more technical standards that OSHA administers and enforces. Therefore, it can be helpful to break the Standard down into its major parts, and outline the requirements of those individual parts in the simplest possible terms. Those parts include:
- Respiratory protection program 134(c)
- Selection of respirators 134(d)
- Medical evaluation 134(e)
- Fit testing 134(f)
- Use of respirators 134(g)
- Maintenance and care of respirators 134(h)
- Breathing air quality and use 134(i)
- Identification of filters, cartridges, and canisters 134(j)
- Training and information 134(k)
- Program evaluation 134(l)
- Recordkeeping 134(m)
Let’s take a look at each of these parts to better understand our obligations, and how to most effectively and efficiently achieve compliance.
Respiratory Protection Program 1910.134(c)
In any workplace where respirators are necessary or whenever respirators are required by an employer, the employer must establish and implement a written, worksite-specific respiratory protection program. At a minimum, your written program elements must clearly define (where applicable):
- Procedures for selecting appropriate respirators
- Systems for providing medical evaluations to employees who use respirators
- Fit testing procedures for respirators
- Procedures for proper use of respirators during routine work activities and emergencies
- Procedures and schedules for maintaining respirators
- Procedures to ensure adequate air quality, quantity and flow for supplied air respirators
- Training for employees in respiratory hazards and the proper use of respirators
- Procedures for evaluating the effectiveness of the program
The Challenge: Like other OSHA-required written health and safety plans and programs, your written respiratory protection program must be made available to employees and it must be updated whenever changes in workplace conditions or respiratory hazards affect respirator use. All too often, written programs are printed out, filed in a drawer, and rarely ever again see the light of day. In fact, failure to establish and maintain a worksite-specific written program is one of the most frequently cited provisions of OSHA’s Respiratory Protection Standard.
It’s also important to remember that if workers voluntarily use respirators even when not specifically required under the Standard, employers must still do a couple things:
- Provide employees with the Respiratory Protection Standard Appendix D "Information for Employees Using Respirators When Not Required Under the Standard”
- Develop written respiratory protection program elements to ensure (at a minimum) that employees are medically able to use a respirator (i.e. medical examinations), and that the respirators are maintained in a safe condition
Best Practices for Compliance: Maintaining your written program electronically so that it can be easily accessed, edited and distributed throughout the workplace not only streamlines compliance with the standard’s written program requirements contained in 1910.134(c), but it facilitates greater levels of employee participation and engagement when it comes to developing, implementing and reviewing your program.
For workers who participate in voluntary respirator use, you’ll also need to establish a system for tracking which employees are using respirators in order to ensure they are provided with the required information and medical evaluations. For example, when a worker wants to voluntarily use a respirator, ask them to complete a Release Form for Voluntary Respirator Use that requires an employee to acknowledge that they have received the information and understand their right to medical examination under the Standard. With that form in-hand, you can track which employees are voluntarily using respirators and schedule the required initial medical exams.
However, this can quickly become unmanageable as the number of employees participating in voluntary respirator use increases. A more sustainable approach is to collect and manage this information electronically, and develop a system to be actively notified when employees are participating in a voluntary respirator use program.
Selection of Respirators 1910.134(d)
Choosing the respirator that is appropriate for workplace respiratory hazards is essential to protecting workers, but with so many potential respiratory hazards that may be encountered on-the-job and just as many respirator options available to employers, how do you choose the right one?
The Challenge: It all starts with quantitative evaluation of respiratory hazards. OSHA’s Small Entity Compliance Guide for the Respiratory Protection Standard provides valuable clarification on what employers must evaluate when determining the appropriate respirator, but it ultimately boils down to identifying which substances and work activities involving those substances have the potential to create respiratory hazards in the workplace, then performing air sampling and monitoring in areas where those substances or activities are present to quantify exposure levels. From there you can select the correct NIOSH-certified respirator that is appropriate for the chemical state and physical form of the contaminant.
Best Practices for Compliance: Make sure that you maintain a complete and up-to-date inventory of the chemicals present in your workplace. With that inventory in-hand, you can then determine which of those chemicals have any potential respiratory hazards, or if they are regulated by OSHA substance-specific standards and have OSHA-defined permissible exposure limits (PELs). This includes products that contain multiple ingredients of which one or more could expose workers to respiratory hazards.
In addition to the Respiratory Protection and other substance-specific standards, OSHA’s General Duty Clause requires employers to protect workers from all hazardous substances, even those not specifically regulated by OSHA. For those hazardous substances without OSHA substance-specific standards and PELs, you should reference NIOSH, AIHA, ECHA, ACGIH or other published occupational exposure limits (OELs) to determine when a respirator is required. Also, be sure to refer to your chemicals’ safety data sheets (SDSs) to assess potential workplace respiratory hazards, and to determine the toxicity and any OEL for a particular substance.
Once you’ve identified which substances you need to evaluate for respiratory hazards, be sure to collect air samples according to the sampling protocols defined in any applicable substance-specific standards. It’s important to remember that not all hazardous substances that may be used in your workplace are regulated by a specific standard, and therefore do not have a prescribed sampling protocol or OSHA-defined PEL. For substances without specific sampling protocols, be sure to perform workplace air sampling under the worst-case exposure conditions to be sure that you are providing the greatest level of protection for your employees, and also remember to sample from multiple locations within the work area to obtain the most reliable monitoring results.
You’re going to need a data management system to store and analyze your sampling data, and to document compliance with monitoring protocols and requirements. As you can imagine, the greater number of samples you must collect, work areas you must monitor and respiratory hazards present in your workplace, the more complex this task becomes.
The VelocityEHS Industrial Hygiene (IH) solution offers a purpose-built software system specifically designed to handle large volumes of complex IH sampling data, and makes it easy to enter, access, and analyze exposure levels to ensure you’ve fully identified all workplace respiratory hazards. From there, you can more easily identify and select the correct respiratory PPE required to protect workers from those hazards.
Medical Evaluation 1910.134(e)
Employer’s must perform medical evaluations to determine an employee’s ability to use a respirator before they are fit tested or required to use a respirator in the workplace. As part of that evaluation, a physician or other licensed health care professional (PLHCP) must meet with the employee and document the information specified in the Respiratory Protection Standard Appendix C, Part A Sections 1-2. In addition to these initial medical evaluations, there are some other requirements employers need to know, including:
- If seasonal or temporary employees are required to wear a respirator, you must provide them with all required medical evaluations for the duration of their employment
- Any PLHCP may administer the required medical questionnaire/medical examination as long as such an examination is within the scope of their medical license. Check with PLHCPs in your area to identify qualified PLHCPs, or contact your state medical licensing board
- If an employee refuses to be medically evaluated for the use of a respirator, he or she CANNOT be assigned to a job that requires use of a respirator
- You must schedule a follow up medical examination for employees who answer “Yes” to any of questions 1-8 in Appendix C, Part A Sections 2, or whose initial medical examination otherwise demonstrates the need for a follow-up medical examination
- Employers must provide the PLHCP with supplemental information necessary to make an accurate determination of an employee’s ability to use a respirator, including:
- The type and weight of the respirator to be worn by the worker
- The duration and frequency of respirator use (including use for rescue and escape)
- The worker’s expected level of physical effort required to perform tasks while wearing a respirator
- Additional personal protective clothing and equipment that the employee would be expected to wear in the performance of work tasks
- The temperature and humidity extremes that may be encountered in the work environment where respirator use is required
- A copy of your written respiratory protection program
- A copy of OSHA’s Respiratory Protection Standard
- Employers must provide additional medical evaluations for employees who use respirators whenever:
- The employee reports symptoms related to his or her ability to use a respirator
- The PLHCP, respiratory protection program administrator or supervisor, determines that a medical re-evaluation is necessary
- Information from the respiratory protection program suggests a need for re-evaluation (i.e. respirator use or respiratory hazards change)
- Workplace conditions (such as protective clothing, temperature, or level of work effort) have changed, resulting in an increased physiological burden on the employee
- The results of a medical examination and PLHCP recommendations suggest that additional medical evaluations are necessary
The Challenge: Failure to provide medical evaluations to workers who wear respirators in the workplace is another of the most common provisions cited by OSHA inspectors under the Respiratory Protection Standard. It’s important for employers to remember that beyond employees’ initial medical evaluations, there are numerous other workplace conditions that trigger the need to provide employees with subsequent exams.
To ensure all required medical examinations are being performed for all employees in your workplace, you need the ability to accurately track employee respirator use. From there you can identify which employees must receive exams, and then determine when they must be performed. You also need to document and review PLHCP recommendations following medical evaluations, and continually evaluate any changes in respiratory hazards or other workplace conditions that would prompt follow up medical exams. Lastly, you need to establish a system to maintain and monitor this information in order to ensure that you are providing medical evaluations as they are required.
Best Practices for Compliance: A good place to start is enrolling employees who wear respirators in a medical surveillance program. A medical surveillance program offers employers a systematic framework for documenting workplace respiratory hazards, monitoring employee respirator use, tracking employee medical examination requirements, and scheduling those exams to more easily identify workers who require medical evaluations to verify compliance. Even though it is not specifically required under OSHA’s Respiratory Protection Standard, many of OSHA’s substance-specific standards do require medical surveillance and even medical removal of employees if certain exposure conditions are met.
VelocityEHS Industrial Hygiene (IH) solution not only provides an easy-to-use tool for evaluating workplace respiratory hazards and assessing respiratory protection requirements, but it also offers an integrated medical surveillance program management tool that simplifies the enrollment or removal of personnel from medical surveillance programs, and allows you to easily schedule and track exams to quickly determine which employees need them and when, and if medical removal requirements are triggered based on employee exposure.
Fit Testing 1910.134(f)
Before an employee can be required to use any respirator with a negative or positive pressure tight-fitting facepiece, the employee must be fit tested for that respirator. After the initial fit testing, subsequent fit tests must be performed at least annually, and whenever an employee switches to a different type of tight-fitting facepiece respirator. Guidance on which types of respirators require fit testing can be found in OSHA’s Small Entity Compliance Guide for the Respiratory Protection Standard. If any of these types of respirators are used in your workplace, you must meet the requirements under this part of the Standard.
Appendix A of the Respiratory Protection Standard contains OSHA’s approved fit test protocols, which are the testing methods and evaluation criteria employers are permitted to use when performing fit tests. There are a variety of approved protocols, and they represent some of the more technical aspects of the Respiratory Protection Standard. In fact, on October 1, OSHA published issued a final rule approving two new alternative fit testing protocols to supplement the four existing quantitative fit testing protocols already listed in Appendix A of the Respiratory Protection Standard. Employers should take some time to familiarize themselves with the details of these fit test protocols to ensure fit tests are performed accurately and in compliance with the Standard.
The Challenge: The variety of approved fit testing protocols listed in Appendix A means that employers have quite a bit of flexibility when it comes to choosing the one that’s right for them. Generally speaking, the fit test protocols you select will be determined the type of respirators used in your workplace, and the test reagents/substances and testing equipment appropriate to those types of respirators. Again, be sure to study Appendix A of the Respiratory Protection Standard to determine which testing protocol is appropriate for the respirators in your workplace.
One of the most difficult parts of compliance with OSHA fit testing requirements is scheduling and sufficiently documenting fit test results for all fit tests performed on all employees who require them, for every covered respirator type used in your workplace. Sounds like a big task, right? The more employees that require the use of respirators, especially temporary workers who are enter and leave the workplace on a frequent basis, the greater this challenge becomes.
Best Practices for Compliance: Employers should consider implementing a software system that coordinates the scheduling, documentation and follow up of your required fit testing protocols and activities. This is particularly true for employers who need to manage fit testing compliance across multiple locations, or for large numbers of employees who use respirators in the workplace. If you can quickly and easily determine which employees use which types of respirators, what fit testing protocols are required for those respirator types, when fit tests must be performed, and then quickly document fit test results, you’ll be well on your way to ensuring compliance with OSHA fit testing requirements.
The VelocityEHS Respirator Fit Test (RFT) solution standardizes the scheduling, documentation and follow up of your RFT activities, giving you a powerful platform for managing RFT requirements across multiple locations and large numbers of employees. You can easily determine which employees use which types of respirators, schedule and assign fit tests, and record results to easily demonstrate compliance. Built-in OSHA-approved testing protocols and a complete library of pre-test procedures make it easy to select and perform the right RFT protocols for the respirator types used in your workplace.
In Part Two of our discussion on OSHA’s Respiratory Protection Standard, we’ll finish our walk-through of the remaining parts of the Standard. We’ll also take a brief look into how some of the OSHA substance-specific standards mentioned earlier overlap with the Respiratory Protection Standard, and begin to think about ways we can condense and simplify those requirements to eliminate redundancies and streamline compliance.
Stay tuned to the VelocityEHS Blog, and be sure to subscribe for the latest EHS management news and best practices.